Where Trauma Is Stored in the Body: A Gentle Guide for Sensitive Nervous Systems
Many people arrive at this question quietly, often late at night: “Where is all of this in me? Where trauma is stored in the body, and is that why I feel this way?”
If that is you, you are not alone.
You may feel like you are “too sensitive,” “too emotional,” or “overreacting,” especially when nothing obvious seems wrong. At the same time, your body continues to send signals—tightness, pain, gastrointestinal issues, exhaustion, or a sense of being on edge. It can be confusing and scary.
In this article, we will explore where trauma is stored in the body in simple language. We will examine how the nervous system retains challenging experiences, how this can manifest as symptoms, and how gentle, body-based work can create space and relief.
Why this question matters when you feel “too sensitive”
Many women and sensitive people are told that their symptoms are “all in their head.” You might have normal blood work and normal scans, but you do not feel normal. You may feel dismissed, unseen, or even doubting your own experience.
Because of this, understanding where trauma is stored in the body can be deeply validating. It offers a different story. Your body is not broken or dramatic. Instead, it has been doing its best to protect you, sometimes for many years.
When we see symptoms as messages from the nervous system, rather than random problems, things begin to make more sense. This shift can bring relief even before anything changes, because you finally have a framework for what you are feeling.
What we really mean by trauma (it is more than big events)
When people hear the word “trauma,” they often think about big, obvious events—accidents, assaults, war, or significant losses. Of course, these are traumatic. But trauma can also come from long, slow experiences that did not look dramatic from the outside.
For example:
- Growing up in a home where emotions were never talked about
- Being praised only when you achieved or were “easy.”
- Feeling responsible for other people’s moods
- Living through chronic illness, money stress, or ongoing tension in relationships
Over time, these experiences can leave the nervous system in a state of constant alert. The body does not get to fully relax. Instead, it stores the “unfinished story” of what never felt safe, seen, or soothed.
This is one way to understand where trauma is stored in the body.
How the nervous system stores trauma in the body
The nervous system’s main job is to keep you alive. It monitors for danger, responds, and, ideally, helps you return to safety. When that does not happen, the energy of the response can stay held in the body.
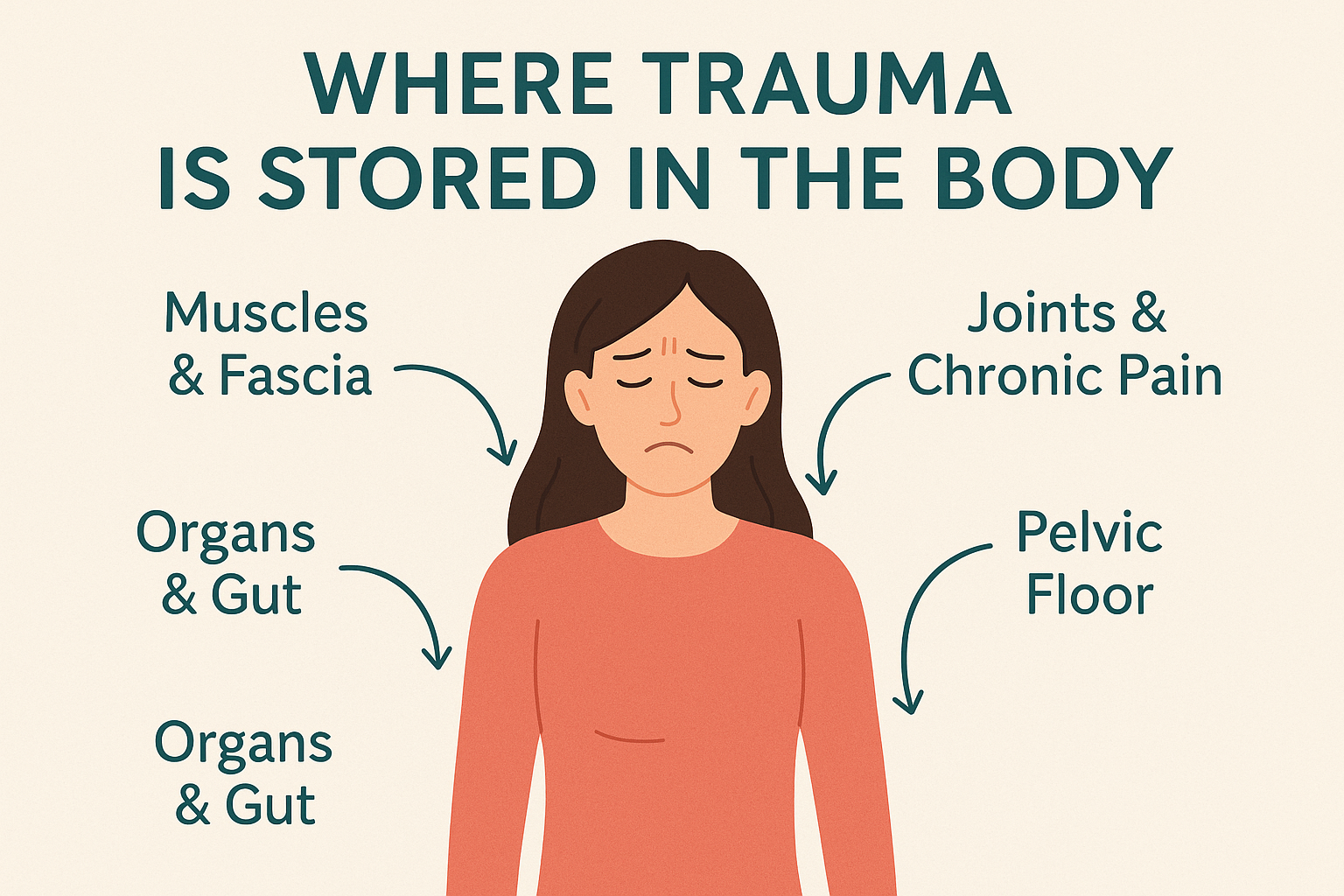
Because everything in the body is connected, trauma can be stored in many places at once. Muscles, fascia, organs, joints, and even posture can all reflect what the nervous system has lived through.
Below are some common ways this can show up. These are not diagnoses. Instead, they are gentle lenses that may help you understand your own patterns a little more kindly.
Muscles and fascia: the body’s memory fabric
Fascia is the thin, web-like tissue that surrounds muscles, organs, and bones. You can think of it like the body’s memory fabric. When the nervous system stays on guard, fascia and muscles can become tight, dense, or “stuck.”
You might notice:
- Chronic neck or shoulder tension that never fully releases
- A heavy, rounded posture, as if you are bracing
- Unexplained aches that move around or flare during stress
These patterns can be part of where trauma is stored in the body. The tissue is not trying to punish you. Instead, it may be trying to hold you together, to keep you safe in a way that once made sense.
Organs and the gut: when emotions land in digestion
Many people feel their emotions in their gut. Maybe your stomach twists before a hard conversation, or you rush to the bathroom when you feel anxious. For some, this becomes a persistent pattern—bloating, cramping, constipation, diarrhea, or a combination of these.
The gut is deeply connected to the brain and nervous system. When the body has experienced ongoing stress or trauma, digestion often slows or accelerates to cope. Over time, this may present as irritable bowel symptoms, food sensitivities, reflux, or nausea.
If this is you, it does not mean you are imagining things. Your gut may be one of the main places where your body has learned to hold stress. In other words, it can be one of the places where trauma is stored in the body and expressed through symptoms.
Joints, headaches and chronic pain patterns
Trauma can also show up in joints and chronic pain. You may have pain that moves, flares without an apparent injury, or lingers long after tissue should have healed. Conditions like fibromyalgia or chronic widespread pain often have a strong nervous system and trauma component.
You might notice:
- Pain that worsens during emotional stress or after conflict
- Headaches that come on when you feel overwhelmed
- Flare-ups after times you “push through” your limits
Again, this does not mean the pain is “all in your head.” Instead, your nervous system may be amplifying pain signals because it is already in a state of heightened alert. The body is trying to say, “Something is too much,” even if you cannot see the original cause.
The pelvis and pelvic floor: holding shame and boundary violations
For many people, especially women, the pelvis and pelvic floor can be a key area where trauma is held. This can be related to birth experiences, sexual trauma, medical procedures, or years of feeling unsafe in relationships or in your own body.
Common experiences can include:
- Pelvic pain or pressure without a clear medical cause
- Pain with intimacy
- Urinary urgency, leaking, or difficulty relaxing
- A feeling of “numbness” or disconnection from the pelvis
Because this area is intimate, many people feel ashamed talking about it. As a result, the body may carry the story alone for a long time. Gentle, trauma-informed work can help this area feel safer again, at your pace.
Signs trauma may be stored in your body
Everyone is unique, and no single sign proves that trauma is stored in the body. However, there are common patterns. You might recognize yourself in some of these:
- You feel “on edge,” even when life looks fine from the outside
- You have symptoms that move around or change, especially with stress
- You swing between doing everything and feeling completely shut down
- Rest never feels truly restful; you wake up tired or wired
- Medical tests keep coming back “normal,” yet you know something is wrong.
- You feel a deep sense that your body is carrying more than you can explain.
If any of this feels familiar, it is understandable to wonder where trauma is stored in the body for you. In my experience, the answer is typically “in more than one place,” and it is always associated with the nervous system.
If some of this sounds familiar, it may be a relief to know you are not imagining things. If you live in Ottawa and would like gentle support, you are welcome to explore working together when and if it feels right.
Why talking about it is not always enough
Talk therapy can be incredibly helpful. It can offer understanding, language, and support. At the same time, some people find that even after years of talking, their body still feels stuck.
This is not a failure. It is simply a sign that the body must also be included in the healing process. Because trauma is often stored in sensation, tension, posture, and reflexes, the body sometimes needs gentle, direct support to shift.
When we invite the body into the conversation, we are not trying to “force” it to let go. Instead, we are offering safety, time, and attention so that the nervous system can update its story.
Gentle ways to begin releasing stored trauma
Every nervous system is different. There is no single right way to heal. However, there are some gentle practices and supports that can help many people.
Starting with safety and pacing
Before anything else, your system needs to feel as safe as possible. This does not mean life has to be perfect. Instead, it means we move slowly enough that your body does not feel pushed or flooded.
Small steps might include:
- Noticing one place in your day where you feel even a little more at ease
- Short, regular pauses to check in with your body
- Choosing practitioners who respect your pace and your “no”
When we honour your limits, your nervous system can gradually trust that it no longer has to be on constant high alert.
Tracking sensations instead of stories
Another gentle practice is learning to notice body sensations without forcing change. For example, you might place a hand on your chest and notice the weight of your hand, the temperature of your skin, or the rhythm of your breath.
Initially, this may feel strange. However, over time, it helps bridge the gap between the mind and the body. This bridge is often where stored trauma begins to soften, because sensations finally have space to be felt and move.
Small, supported movements
Very small movements can be powerful when the nervous system is overwhelmed. This might include gently rolling your shoulders, rocking your pelvis while sitting, or pressing your feet into the floor and then releasing.
The goal is not exercise or performance. Instead, it is to give your body a way to complete some of the responses that were interrupted in the past—like the urge to push away, run, curl up, or stand your ground.
Breath, sound and the vagus nerve
Simple breath and sound practices can support the vagus nerve, which plays a big role in helping the body shift from “fight or flight” into “rest and digest.” For example, longer exhales, gentle humming, or slow sighs can sometimes help the body feel slightly more settled.
These practices should always feel optional and adjustable. If anything feels activating, it is okay to stop. Listening to your body is more important than doing a technique “correctly.”
Gentle touch and bodywork
For some people, working with a trauma-informed practitioner who uses gentle touch can be very supportive. This might include light pressure on specific points, subtle work with fascia, or positions that allow the body to safely unwind tension.
Because your nervous system leads this work, sessions often feel quiet and spacious. The aim is not to “fix” you, but to listen to what your body is ready to release, and what still needs more time.
Support, community and kindness toward yourself
Healing stored trauma is not a quick project. It is a slow, living process. Having kind, attuned support—whether through therapy, bodywork, community, or trusted friends—can make a big difference.
Most of all, it helps to remember that nothing about this is your fault. Your body has been doing what it needed to do to help you survive. Now, little by little, it can learn that more is possible.
How I work with stored trauma in the body at Capital Osteopathy
In my work at Capital Osteopathy in Ottawa, I combine gentle, nervous-system-led osteopathy with functional medicine and applied kinesiology. Most of the hands-on treatment is very soft. There is no cracking, and no forcing the body to change.
Instead, I use acupressure-style contact, subtle testing, and careful listening to follow your body’s signals. Your nervous system sets the pace. Together, we explore where your system is holding tension or old patterns, and we support it to release only what feels ready.
Because trauma can be stored in many places in the body, sessions may include:
- Supporting the gut and digestion
- Helping the body feel the ground and support beneath it
Alongside the hands-on work, we may also talk about simple home practices, nervous-system education, and, when appropriate, functional medicine testing that can reveal hidden stressors in the body.
Further gentle resources
If you would like to keep exploring where trauma is stored in the body and how it connects to your symptoms, you may also enjoy:
- Gut Health and Trauma: The Complete Guide – how the gut, brain and trauma interact
- Interoception: Understanding Its Significant Impact on Mental and Physical Health – how you notice signals inside your body
- Understanding Polyvagal Theory: Enhancing Your Well-Being – a simple map of your nervous system states
- Best 3 Proven Strategies for Managing Nervous System Dysregulation – practical tools to support regulation
- Intergenerational Trauma and Chronic Pain: Unravelling the Hidden Connection – how patterns can be carried across generations
A gentle next step (only if it feels right)
If reading about where trauma is stored in the body feels like it is describing your experience, you are not alone. Many women and sensitive people in Ottawa share similar stories of “normal” tests, long-term symptoms, and a sense that their body is carrying more than anyone can see.
You do not have to figure this out on your own. If it feels right, you are welcome to book a free 15-minute Discovery Session. In this short, no-pressure call, we can explore what you have been living with, answer your questions, and see together whether this kind of gentle, nervous-system-led care might be a fit for you.
And if now is not the time to reach out, that is okay too. Simply understanding where trauma is stored in the body and seeing your symptoms as meaningful can be an essential step in itself. Your body has reasons for feeling the way it does. Those reasons warrant careful consideration.
Disclaimer
The information provided on this website is for educational purposes only and is not intended to diagnose or treat any disease. Please do not apply this information without first speaking with your doctor.